 Anesthesia is a common part of surgeries and other medical procedures and these allow you to temporarily lose sensation. You can have a local, regional, or general anesthetic. General anesthesia will bring a loss of consciousness but can lead to complications. Regional anesthetics can be combined with sedation and blocks sensation from a particular area. Epidurals and spinal blocks are regional anesthetics that can be recommended for surgeries in the lower extremities, pelvis, or lower abdomen.But what is the difference between epidural and spinal block?
Anesthesia is a common part of surgeries and other medical procedures and these allow you to temporarily lose sensation. You can have a local, regional, or general anesthetic. General anesthesia will bring a loss of consciousness but can lead to complications. Regional anesthetics can be combined with sedation and blocks sensation from a particular area. Epidurals and spinal blocks are regional anesthetics that can be recommended for surgeries in the lower extremities, pelvis, or lower abdomen.But what is the difference between epidural and spinal block?
What Is Epidural Block?
Epidural anesthesia is when a hollow needles as well as a flexible and small catheter is inserted between the spinal cord’s outer membrane and the spinal column within the lower or middle back. This area is numbed using a local anesthetic; the needle is then inserted and removed once the catheter passes through it. Then the anesthetic can be injected through the catheter, numbing the surrounding area. Doctors secure the catheter to make it easy to give more medicine if necessary.
What Is Spinal Block?
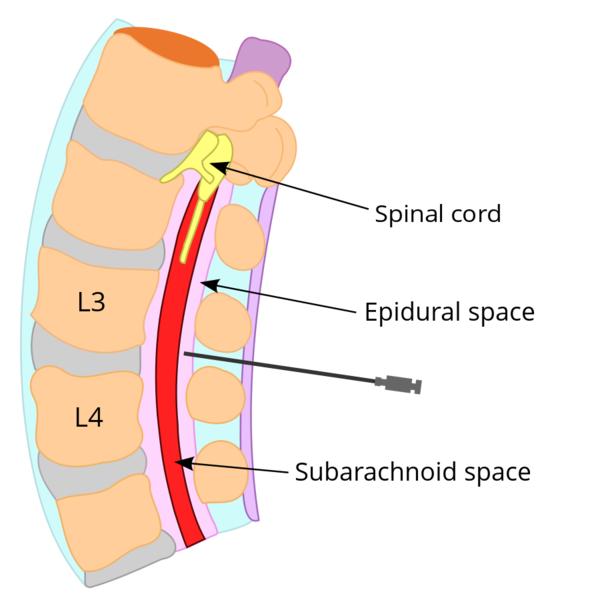
Spinal anesthesia is similar to epidural anesthesia but the injection occurs with a needle that is much smaller. Additionally, the injection goes straight into cerebrospinal fluid surrounding the spinal cord and the procedure is frequently done without a catheter. The dose and technique determines the area that is numbed. In some cases a spinal catheter will be inserted and left to make it easy to administer more medicine.
What Is the Difference Between Epidural and Spinal Block?
Both epidurals and spinal blocks will bring on the loss of body sensation, there are several important differences. The most crucial differences between these two forms of anesthesia are in terms of the duration that the effect lasts for as well as the way they are administered.
1. The Injection Spot and Approach of Administration
Using a spinal block will involve injecting the local anesthetic directly into the subarachnoid space which holds the cerebrospinal fluid. This fluid transports waste and nutrients and acts as a cushion. You can use a small amount of local anesthetic for a spinal block because it spreads easily in the spinal fluid. It is injected using a small needle which is then removed and takes 5 to 20 minutes to complete this process.
The epidural begins differently as the patient has to lie down so the area can be cleaned. More local anesthetic is needed than with a spinal block because it takes more to spread throughout tissues and you also need to intravenously administer fluids. Doctors insert a special need in the epidural space and then place a small catheter inside it before removing the needle and leaving the catheter. This way you can get a continuous dose (as opposed to with a spinal block where there is only one dose). It takes a bit longer as well at 10 to 25 minutes.
2. Effects
Spinal blocks are more commonly used for shorter, simpler procedures while epidurals are used for longer ones. The anesthetic in a spinal block will be felt very quickly and it is strong. Epidurals take 10 to 20 minutes to kick in and still allow for sensation, but no pain. The catheter used with epidurals also makes it easier to give narcotics and anesthetics for postoperative pain.
Spinal blocks are common for procedures with the lower abdominal region or lower limbs. Epidurals are most common for pregnant women in labor or having a C-section, but can also be used for gastrointestinal surgeries. Conversely, a spinal block is also an option for C-sections.
3. Side Effects
Most of the time side effects will be avoided, but they can occur. Spinal blocks may cause low blood pressure, headaches, or back pain. It is more common for complications to happen if the needle is placed in a spinal nerve and damages the nerve fibers. Very rarely this can lead to an infection or even seizures, but this is incredibly rare, especially when the technique is correct.
Epidurals are considered safe but you can have complications related to anesthesia. An example would be if the catheter tip goes in a vein and causes the anesthetic to go into blood vessels. This may lead to heart rhythm disturbances or seizures. A dural puncture (a puncture of the dura) can lead to headaches. Other complications may occur if a hematoma compresses the nerves within the epidural space.
Here is a video to show you the animated review of technique of epidural anesthetic administration, as used in childbirth:
Advantages and Disadvantages of Having an Epidural or a Spinal Block
1. Epidural Block
- Advantages
This is the best way to get pain relief while in labor and it makes it easy to give another dose if you need it. Although you can still feel contractions, you won’t be in pain and it can even help lower high blood pressure. It has the added benefit of being easy to add more anesthetic in the case of a C-section.
- Disadvantages
It takes longer than most methods with 20 minutes for insertion and then 20 more to work. Some women (one in eight) won’t get enough relief and need another method. It may also lead to shivers, itching, or fever. You also can’t walk because the legs will be weak and heavy and you will need help going to the bathroom. It can also increase the length of the pushing stage of labor and increase the chances that your baby needs help coming out with forceps.
2. Spinal Block
- Advantages
It will provide complete pain relief in only several minutes and only a small quantity of the medicine will reach your baby.
- Disadvantages
During the procedure you will need to maintain a somewhat awkward position. You will also need constant fetal monitoring and an IV. The reduced sensation can increase the length of time it takes you to push out your baby or require forceps (as with epidurals). Narcotics can lead to itchiness and you may have a temporary drop in blood pressure or some soreness at the injection site for a few days.